How iMS Cells from Human Fat Are Changing Medicine
Imagine a world where healing is not just a hope, but a reality, thanks to the power of our bodies. In the field of regenerative medicine, a groundbreaking discovery has emerged, one that might sound like science fiction but is very much a scientific fact. Researchers have found a way to transform ordinary human fat cells into “smart” stem cells, known as Induced Multipotent Stem Cells (iMS). This breakthrough, led by a team at UNSW Sydney, is not just a step, but a giant leap in the field of medical science.
These iMS cells are not your ordinary stem cells. They are akin to chameleons, with an uncanny ability to adapt and transform based on their environment. This means they have the potential to repair various types of tissue damage, heralding a new era in treating injuries and diseases. What’s more intriguing is that these cells come from a source most of us would love to spare – human fat. This discovery could change how we view our bodies and their healing capabilities.
But how does this work? And what makes these iMS cells so special and different from other stem cell technologies? In this article, we delve into the fascinating world of iMS cells, exploring their potential, the science behind their creation, and what the future holds for this innovative approach to healing.
What Makes iMS Cells Unique?
iMS cells, or Induced Multipotent Stem Cells, represent a significant advancement in stem cell research. Developed by a team at UNSW Sydney, these cells are derived from human fat, a resource that is both abundant and easily accessible. But what sets them apart from other stem cells is their extraordinary adaptability.
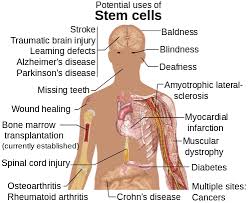
iMS cells are like the chameleons of the cellular world. They possess the unique ability to respond to their environment and transform into the type of tissue needed for repair. This adaptability is a game-changer in regenerative medicine, as it means these cells can potentially heal a variety of tissues – from muscle to bone to nerve cells.
The Process of Creating iMS Cells
Creating iMS cells involves reprogramming adipocytes (fat cells) using a specific compound mixture. This process, intriguingly, is similar to erasing the cells’ original identity, turning them into a blank slate ready to adapt and transform. The mixture used includes azacitidine, a drug typically used in blood cancer therapy, and a growth factor that stimulates cell regeneration. Within about three and a half weeks, the fat cells lose their lipid content and become iMS cells.
The fascinating part? When these reprogrammed cells were tested in animal models, they remained dormant until an injury occurred. Once activated by the injury, they transformed into the required tissue type, effectively demonstrating their ability to adapt to different healing needs.
The Advantages and Potential of iMS Cells in Healing
One of the most remarkable aspects of iMS cells is their versatility. Unlike traditional stem cell therapies, which often have limitations in the types of tissues they can regenerate, iMS cells can adapt to a wide variety of tissue types. This versatility opens up new possibilities in treating various injuries and diseases, from repairing damaged muscles to regenerating nerve cells.
Safety and Personalization
Another significant advantage of iMS cells lies in their safety and patient-specific nature. Since these cells are derived from an individual’s own fat, the risk of rejection is dramatically reduced compared to other stem cell therapies. Moreover, in animal studies, iMS cells have shown no signs of unwanted tissue growth, such as tumor development, which has been a concern with other stem cell technologies. This safety profile makes iMS cells a promising candidate for future therapeutic applications.
Application in Clinical Settings
The potential applications of iMS cells in clinical settings are vast. For instance, in muscle injury models, iMS cells have specifically contributed to the regeneration of satellite cells and myofibers, showcasing their ability to target specific areas of damage. Their context-dependent regenerative capacity implies that they could be tailored for various types of tissue repair, making them a versatile tool in the medical toolkit.
Reprogramming Fat Cells: The Journey to Smart Stem Cells
The Transformation of Adipocytes
The process of converting adipocytes, or fat cells, into iMS cells is a fascinating journey of cellular transformation. It begins with exposing the fat cells to a compound mixture, primarily azacitidine and a growth factor. Azacitidine is not just any compound; it’s a drug commonly used in blood cancer therapy, known for its ability to influence cell behavior.
The Role of Azacitidine and Growth Factors
Azacitidine plays a crucial role in this transformation. It works by reprogramming the genetic material of the fat cells, essentially resetting their identity. Accompanying azacitidine, the growth factor stimulates the cells to grow and repair tissue. This combination effectively convinces the fat cells to shed their original function and embrace a new role as multipotent stem cells.
From Fat to iMS Cells
The transformation is not instantaneous. It takes around three and a half weeks for the fat cells to discard their lipid content and fully lose their identity as adipocytes. Once this process is complete, what emerges are iMS cells, primed and ready to adapt to various tissue types for repair.
Practical Applications and Devices
In practical terms, this reprogramming can be done in two ways. The first method involves placing a patient’s fat cells in a device where they incubate with the compound. Alternatively, a mini pump could be used directly in the body, ideally placed near the part that needs repair. This pump would dispense regulated doses to create new, smart stem cells on site.
Future Perspectives: Bridging the Gap from Laboratory to Clinic
While the results from animal studies are promising, translating these findings to human therapies is a complex and meticulous journey. This path involves extensive research, preclinical studies, and clinical trials to ensure the safety and efficacy of iMS cell therapies in humans. The process is rigorous and often lengthy, potentially spanning up to 15 years. This timeline accounts for the inherent challenges and setbacks that are common in medical research.
The Importance of Rigorous Research
The thorough research required before iMS cells can be used in human treatments is crucial for several reasons. It ensures that the cells are safe and effective for various types of tissue repair in humans, and it helps in understanding the long-term implications of such treatments. Additionally, this research will provide insights into optimizing the reprogramming process and the best ways to apply these cells in clinical settings.
Exploring Histone Modifications and CpG Methylation
An interesting aspect of this future research involves understanding the similarities and differences between adipocyte-derived iMS cells and other types of stem cells, like adipose tissue-derived mesenchymal stem cells. This comparison is vital in understanding how iMS cells function and their potential advantages or limitations. Specifically, studying aspects like histone modifications and CpG methylation in these cells could provide deeper insights into their behavior and efficiency.
Cutting-Edge Technologies Enhancing Research
The advancement of stem cell therapies, including iMS cells, is heavily reliant on technological innovations. From sophisticated imaging technologies to advanced genetic sequencing, these tools play a crucial role in understanding, developing, and applying stem cell therapies. Emerging technologies like artificial intelligence and machine learning are also becoming integral in analyzing complex biological data, potentially speeding up research and discovery.
The Future of Personalized Medicine
iMS cells represent a significant step towards personalized medicine, a field that aims to tailor medical treatments to individual patients. This approach could revolutionize how we treat a myriad of conditions, offering therapies that are specifically designed based on a person’s unique genetic makeup, lifestyle, and environment. The intersection of stem cell research with personalized medicine promises not only more effective treatments but also the potential to prevent diseases before they manifest.
Despite the challenges and the long road ahead, the advent of iMS cells represents a significant leap forward in regenerative medicine. The possibility of using a patient’s own tissue to create versatile, safe, and effective stem cells for tissue repair is an exciting prospect. While it’s important to remain grounded in the realities of medical research, the potential of iMS cells to revolutionize healing and tissue repair offers a glimpse into a promising future.
Key Insights and Tips on iMS Cells and Regenerative Medicine
The field of regenerative medicine is rapidly evolving. Keep up with the latest research and developments, especially regarding iMS cells and their applications.
Understanding the Source:
Remember that iMS cells are derived from human fat cells. This source is not only abundant but also means that therapies developed from these cells are less likely to be rejected by the patient’s body.
The Role of Patient-Specific Treatments:
Emphasize the importance of personalized medicine. iMS cells offer a route to treatments that are tailored to the individual, reducing the risk of complications.
Safety First:
Be aware of the rigorous safety protocols in place for developing iMS cell therapies. These protocols are crucial to ensure the treatments are safe and effective.
Realistic Expectations:
Understand that while the potential of iMS cells is enormous, the path from research to clinical application is long and complex. It’s important to have realistic expectations about the availability of these treatments.
Ethical Considerations:
Keep an eye on the ethical aspects of stem cell research. As with any medical advancement, ethical considerations play a vital role in how these therapies are developed and implemented.
Potential Applications:
Stay curious about the various potential applications of iMS cells, from healing wounds to treating chronic diseases. The versatility of these cells opens up numerous possibilities in medicine.
Community and Support:
Engage with communities and support groups focused on regenerative medicine. Sharing knowledge and experiences can be beneficial for both patients and researchers.
Advocacy and Awareness:
Advocate for and contribute to awareness about the importance of stem cell research and its potential to transform healthcare.
Continual Learning:
Finally, encourage continual learning and curiosity. The field of regenerative medicine is constantly advancing, and staying informed is key to understanding its future impact.
Ethical and Regulatory Considerations in Stem Cell Research
Stem cell research, especially advancements like iMS cells, is often at the forefront of ethical discussions. It’s crucial to address the ethical implications of using human-derived cells for medical purposes. This involves considering patient consent, the source of the cells, and the purpose of the research. Ensuring ethical integrity in this field is not just a regulatory requirement but a moral imperative to maintain public trust and support.
Regulatory Hurdles and Approval Processes
In addition to ethical considerations, navigating the regulatory landscape is a significant challenge in bringing iMS cell therapies to the market. Different countries have varying regulations governing stem cell research and therapy. Understanding and complying with these regulations is crucial for researchers and pharmaceutical companies. The approval process for new therapies is rigorous, involving multiple phases of clinical trials and thorough reviews by bodies like the FDA in the United States.
Embracing a New Era in Healing
As we’ve explored the fascinating world of iMS cells, it’s clear that we stand on the brink of a new era in regenerative medicine. The discovery of these ‘smart’ stem cells, derived from human fat, offers a glimpse into a future where healing and tissue repair could be more effective, personalized, and safe.
The journey of transforming adipocytes into iMS cells is not just a scientific achievement; it’s a beacon of hope for those awaiting breakthroughs in medical treatments. The adaptability and versatility of these cells mark a significant departure from traditional stem cell therapies, offering a potential solution to the limitations and risks associated with current methods.
While the path from laboratory to clinical application is long and fraught with challenges, the promise these cells hold is too significant to overlook. The journey of research, trials, and eventual clinical use is a testament to the dedication and ingenuity of scientists and medical professionals worldwide.
As we await the day when these cells can be used in human therapies, it’s important for us all – whether we’re patients, healthcare providers, or simply curious minds – to stay informed and engaged with the progress in this field. The possibilities that iMS cells present are not just a leap in medical science; they are a step towards a future where the power to heal is found within our own bodies.
The post How iMS Cells from Human Fat Are Changing Medicine appeared first on Healthy Holistic Living.